A growing body of research underscores the pivotal role played by the gut microbiota in the human body. The gut microbiota exerts profound influence on energy metabolism, inflammatory responses, and modulation of tumor cell proliferation and differentiation. Its intricate connections with cardiovascular diseases, depression, diabetes, immune function, hyperlipidemia, colorectal cancer, and cirrhosis have become increasingly evident. A healthy gut microbiota contributes to the stability of the intestinal mucosa, facilitates energy intake and metabolism, and enhances the immune system. Conversely, an aberrant gut microbiota can give rise to a myriad of health issues.
In a balanced state of health, the human gut microbiota is a diverse collection of microorganisms, encapsulating entities such as bacteria, viruses, and archaea, among others, of which bacteria are the most abundant. Predominantly, the gut microbiota is a consortium of the bacterial classes Firmicutes and Bacteroidetes, which cooperate to form more than 90% of the total bacterial population. The remaining fraction of the gut microbiota is chiefly composed of Proteobacteria and Actinobacteria species.
Upon ingestion, undigested components of the diet, such as dietary fibers, resistant starch, as well as certain proteins and fats, traverse from the small intestine to the colon. Within the colon, these substances undergo anaerobic fermentation by the intestinal microbiota, giving rise to a spectrum of compounds collectively referred to as gut microbiota metabolites. Primary among these are short-chain fatty acids (SCFAs), trimethylamine oxide (TMAO), bile acids, ethanol, vitamins, and various sulfur-, hydrogen-, and carbon-containing entities.
The enduring symbiosis between humans and the gut microbiota hinges on a dynamic equilibrium. The stability of microbial composition is intricately linked to the composition of these metabolites. Factors such as diet, pharmaceuticals, age, gender, intestinal microenvironment (including factors like intestinal pH and mucosal changes), and diseases have the potential to induce anomalies in both the gut microbiota and its metabolic byproducts.
Creative Proteomics offers targeted services for the detection of gut microbiota metabolites. These include untargeted metabolomics, complete targeted metabolomics, short-chain fatty acids, bile acids, TMAO, and Tryptophan among others.
Select Services
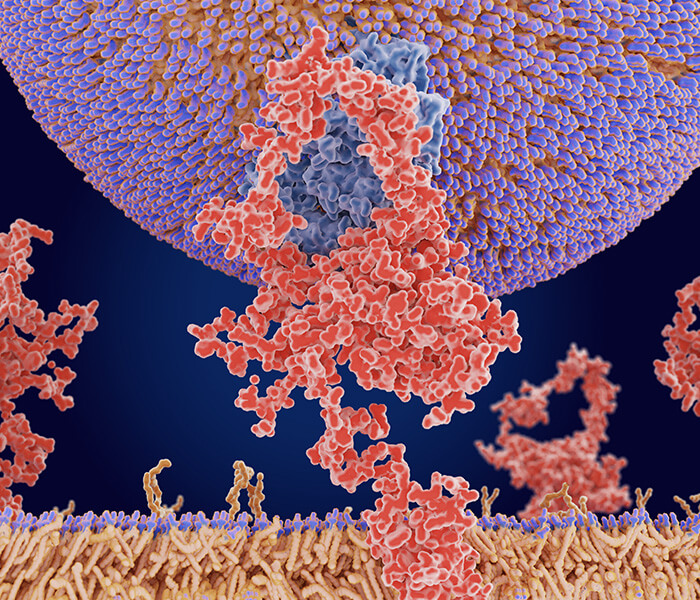
 Figure 1. The Influence of Gut Microbiota Metabolic Products on Host Homeostasis.
Figure 1. The Influence of Gut Microbiota Metabolic Products on Host Homeostasis.
Gut Microbiota Metabolic: SCFAs
Short-chain fatty acids (SCFAs) are organic fatty acids typically characterized by containing less than six carbon atoms in their carbon chains. They include acetic acid, propionic acid, butyric acid, isobutyric acid, valeric acid, isovaleric acid, and caproic acid.
The biosynthesis of Short Chain Fatty Acids (SCFAs) occurs as a result of several enzymatic reactions orchestrated by the gut microbiota. They metabolize a plethora of monosaccharides and oligosaccharides derived from dietary fiber fermentation into SCFAs, including acetic, propionic, and butyric acids. Key processes include:
1) Acetate formation from pyruvate via the acetyl-CoA or Wood-Ljungdahl pathway. 2) Propionate synthesis from succinate via the succinate pathway, resulting in the conversion into methylmalonyl-CoA. 3) Butyrate production through the concatenation of two acetyl-CoA molecules, then reduction to butyryl-CoA, and finally, transformation into butyrate via the phosphotransbutyrylase and butyrate kinase, otherwise known as the classical pathway.
SCFAs exhibit a multitude of functional roles, including energy provision through oxidation, blood sugar regulation, drug release controlling via conjugation with monosaccharide molecules, maintenance of the balance of electrolytes and water, anti-pathogenic microbe and anti-inflammatory actions, regulation of gut microbiota equilibrium, improvement of intestinal function, immune regulation, anti-cancer activities, and gene expression modulation.
SCFAs are primarily produced in the colon, and their variety and quantity depend mainly on the composition of the gut microbiota, transit time within the gastrointestinal tract, host-microbial metabolic flux, and the fibre content in the host's diet. Bacteria genera Bacteroides, Bifidobacterium, Enterococcus, Ruminococcus, Peptostreptococcus, Clostridium, and Streptococcus are the predominant SCFA-producing microflora.
 Figure 2. The Production and Mechanism of Action of Short-Chain Fatty Acids
Figure 2. The Production and Mechanism of Action of Short-Chain Fatty Acids
Gut Microbiota Metabolic: Bile Acids
Bile acids, which are steroidal substances, are categorized into two types: primary and secondary bile acids. Primary bile acids are synthesized and stored in the bile by hepatic cells, while secondary bile acids result from bacterial metabolism. Primary bile acids are produced from cholesterol through two pathways: (1) the classical pathway, where cholesterol is metabolized by CYP7A1 (cholesterol 7α-hydroxylase) within hepatic cells, and (2) the acidic pathway, where cholesterol is metabolized by enzyme CYP27A1 (sterol 27-hydroxylase), located in extrahepatic tissues. Examples include cholic acid (CA) and chenodeoxycholic acid (CDCA) in humans, and muricholic acid (MCA) in mice. Once the primary bile acids are conjugated with glycine or taurine, they form bile salts, and are stored in bile. Upon eating, these bile salts enter the gastrointestinal tract, where approximately 95% of bile acids are reabsorbed and circulate between the liver and intestine. The remaining 5% of bile acids undergo dehydroxylation to form secondary deoxycholic acid (DCA) and lithocholic acid (LCA). Bacteria, particularly those belonging to the phyla Bacteroidetes and Actinobacteria, release an enzyme called bile salt hydrolase (BSH) to hydrolyze the amino acids in the bile salts and thus form secondary bile acids. These bacteria can utilize the resultant amino acids for their growth requirements. Bile acids can regulate various conditions such as Clostridium difficile infection, inflammatory bowel disease, inflammation and cancer, metabolic disorders like metabolic syndrome, among other conditions.
The interaction between the gut microbiota and the metabolism of bile acids, along with the regulatory impact of bile acids on host metabolism, constitutes two pivotal factors in the establishment of the gut microbiota-bile acids-host metabolism axis. The evolving composition of the gut microbiota and the dynamic pool of bile acids present novel avenues for our pathological understanding of the onset and progression of metabolic diseases.
 Figure 3. The impact of host and microbiome-dependent bile acids on human diseases
Figure 3. The impact of host and microbiome-dependent bile acids on human diseases
Gut Microbiota Metabolic: TMAO
Trimethylamine (TMA), an organic compound, is generated by the intestinal microbiota during the metabolism of dietary nutrients that include TMA entities, such as choline, phosphatidylcholine, and L-carnitine. Subsequently, TMA is transported to the liver via the portal venous system, where flavin-containing monooxygenase3 (FMO3) within the liver oxidizes it to generate Trimethylamine N-oxide (TMAO). Research highlights that eight genera within the phyla Firmicutes and Proteobacteria possess the ability to convert choline into TMA. These include Anaerococcus hydrogenalis, Clostridium asparagiforme, Clostridium hathewayi, Clostridium sporogenes, Escherichia fergusonii, Proteus penneri, Providencia rettgeri, and Edwardsiella tarda.
TMAO is identified as a substantial risk factor in the onset of atherosclerosis, thrombosis, and other cardio-cerebrovascular diseases. The levels of TMAO in individuals with cardio-cerebrovascular disease are discernibly higher as compared to those in good health. Therefore, elevated levels of TMAO signify an increased risk for future health complications.
Gut Microbiota Metabolic:Tryptophan
Tryptophan is an indispensable aromatic amino acid, fundamentally characterized by an indole grouping affixed to the beta carbon at the 3rd position in its structure. Despite being the least abundant among the 20 usual amino acids in both proteins and cells, Tryptophan stands significantly at the forefront in terms of molecular weight. It singularly serves as a substantial precursor and host metabolite in microbial biosynthesis. Gut microbiota absorption of Tryptophan plays a pivotal role as it restricts and orchestrates the usage within host cells. Throughout this process, the degradation of Tryptophan generates indole derivatives, broadening its metabolic communication across diverse tissue organs.
Gut microbiota metabolizes tryptophan into indole-containing metabolites, which regulate the host's immune system by activating the aryl hydrocarbon receptor (AHR). AHR functions as a ligand-gated transcription factor in immunoregulation. Tryptophan metabolites stimulate AHR to augment anti-inflammatory responses, thus maintaining homeostasis between the host and gut microbiota. Tryptophan, during its metabolism by the gut microbiota, generates neurotransmitters affecting the host's serotonin activity. Serotonin, a metabolic product of tryptophan, significantly influences the host's biosynthesis and neurotransmitter levels. Additionally, Clostridium sporogenes within the gut metabolize tryptophan into the neurotransmitter tryptamine (TRA).
Metabolic Aspect of Gut Microbiota: Neurotransmitter
Over the course of evolution, gut microbes have fostered a symbiotic relationship with their hosts. The gut microbiota is capable of producing neuroactive metabolites, such as neurotransmitters and their precursors. These metabolites alter the concentrations of related neurotransmitters and precursors in the brain, consequently influencing neuronal activity and cognitive functions either directly or indirectly. Research reveals that mammalian gut microbiota can break down amino acids to generate neuroregulatory compounds, including gamma-aminobutyric acid (GABA, produced by Lactobacillus, Bifidobacterium, and Streptococcus), desaminoadrenaline (produced by E.coli and Bacillus), dopamine (produced by Bacillus), histamine (produced by various bacteria), and serotonin (produced by Streptococcus, E.coli, and Enterococcus). In addition, gut microbiota generate nitric oxide (NO) and bioamines (such as tryptamine and phenylethylamine) during protein degradation. Current research on the impact of these metabolic products on the gut and peripheral tissues is still in its infancy.
References
- Cheng L, Qi C, Yang H, et al. gutMGene: a comprehensive database for target genes of gut microbes and microbial metabolites. Nucleic Acids Res. 2022.
- Koh A, De Vadder F, Kovatcheva-Datchary P, Bäckhed F. From Dietary Fiber to Host Physiology: Short-Chain Fatty Acids as Key Bacterial Metabolites. Cell. 2016.
- Collins SL, Stine JG, Bisanz JE, Okafor CD, Patterson AD. Bile acids and the gut microbiota: metabolic interactions and impacts on disease. Nat Rev Microbiol. 2023.