Neurological disorders, encompassing a broad spectrum of conditions affecting the central and peripheral nervous systems, pose significant challenges to both patients and healthcare providers. Common neurological diseases such as Alzheimer's disease, Parkinson's disease, multiple sclerosis, epilepsy, and amyotrophic lateral sclerosis (ALS) manifest through a myriad of symptoms, impacting cognitive, motor, and sensory functions.
The intersection of neurology with fields like metabolomics and proteomics offers a promising avenue for advancing our understanding and management of neurological disorders. Metabolomics investigates the biochemical processes within cells, providing insights into metabolic dysregulation associated with neurological diseases. Likewise, proteomics examines the expression and interactions of proteins, shedding light on molecular pathways underlying neuronal dysfunction.
Despite remarkable progress in research, diagnosing and treating neurological disorders remains challenging. The intricate nature of the nervous system, coupled with the heterogeneous presentation of symptoms among patients, complicates early detection and personalized treatment strategies. Moreover, the lack of reliable biomarkers and effective therapeutic interventions further underscores the need for innovative approaches in neurology.
Integrating insights from metabolomics and proteomics into the study of neurological disorders holds promise for identifying novel biomarkers, elucidating disease mechanisms, and developing targeted therapies. By fostering interdisciplinary collaborations and leveraging technological advancements, we can strive towards more accurate diagnosis, effective treatment, and improved outcomes for individuals affected by neurological diseases.
Types of Biological Fluids and Their Role in Neurological Disorder Research
Biological fluids are invaluable in the study of neurological diseases. These fluids, which include blood, cerebrospinal fluid (CSF), urine, saliva, and other excretions like tears and sweat, serve as repositories for proteins and metabolites that reflect the physiological and pathological states of the body.
Blood
Blood is a complex fluid comprising plasma and cells, including red blood cells, white blood cells, and platelets. It circulates throughout the body, delivering oxygen and nutrients to tissues and removing waste products. In proteomics and metabolomics research, blood is frequently analyzed due to its accessibility and the comprehensive information it provides about an individual's health status. Blood biomarkers have shown immense potential in diagnosing neurological diseases. For instance, specific protein markers and metabolic profiles in blood have been linked to Alzheimer's disease, offering potential non-invasive diagnostic tools.
Cerebrospinal Fluid (CSF)
CSF is a clear fluid surrounding the brain and spinal cord, playing a critical role in cushioning and protecting the central nervous system. Given its direct contact with the brain, CSF is a prime candidate for studying neurological disorders. Research advancements have identified numerous proteins and metabolites in CSF that are indicative of neurological conditions. For example, elevated levels of tau protein and beta-amyloid peptides in CSF are strongly associated with Alzheimer's disease.
Urine
Urine is a waste product excreted by the kidneys and reflects the body's metabolic processes. Its composition includes various metabolites that can be indicative of an individual's metabolic state. Urine is particularly valuable in metabolomics research due to its non-invasive collection. Metabolic profiling of urine has been used to discover biomarkers for neurological diseases such as multiple sclerosis, where specific metabolites may reflect disease progression and response to treatment.
Saliva
Saliva, produced by salivary glands, contains a mixture of water, enzymes, electrolytes, and proteins. It offers a non-invasive means to collect samples for analysis. Proteins and metabolites in saliva have been studied for their diagnostic potential in neurological disorders. For instance, alterations in salivary cortisol levels have been investigated as potential markers for stress-related conditions such as depression and anxiety.
Other Biological Fluids
Other biological fluids, including tears and sweat, are also being explored for their potential in neurological disease research. These fluids can provide additional insights, particularly when combined with data from blood, CSF, urine, and saliva. For example, tear fluid has been studied for biomarkers related to neurodegenerative diseases, while sweat analysis is being investigated for its potential to monitor metabolic changes associated with neurological conditions.
Select Services
Applications of Proteomics in Neurological Disorder Research
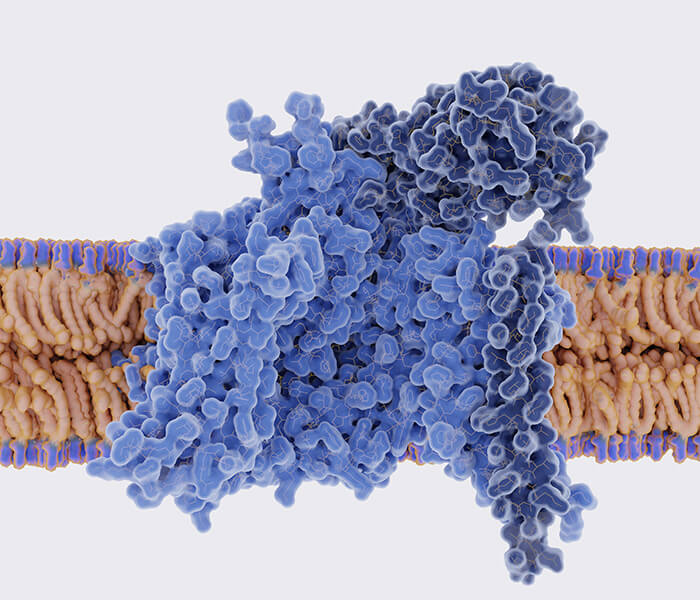
Proteomics, the study of proteins on a large scale, has revolutionized our understanding of neurological disorders by allowing researchers to explore the intricate molecular mechanisms underlying these conditions. Proteomic techniques enable the identification, quantification, and characterization of proteins, providing valuable insights into disease pathogenesis, biomarker discovery, and potential therapeutic targets.
Proteomics Techniques
- Mass Spectrometry (MS): Mass spectrometry is a cornerstone technique in proteomic research, allowing for the identification and quantification of proteins within a sample. In the context of neurological disorders, MS facilitates the analysis of protein expression levels, post-translational modifications, and protein-protein interactions. By comparing the proteomic profiles of healthy and diseased tissues or biofluids, researchers can pinpoint aberrant protein patterns associated with specific neurological conditions.
- Two-Dimensional Gel Electrophoresis (2-DE): Two-dimensional gel electrophoresis is a powerful method for separating complex protein mixtures based on their isoelectric point and molecular weight. This technique enables the visualization of thousands of proteins simultaneously, providing researchers with a comprehensive overview of the proteome. In neurological disorder research, 2-DE has been instrumental in identifying disease-specific protein signatures and unraveling the molecular mechanisms underlying pathogenesis.
Discovery and Validation of Protein Biomarkers
One of the primary applications of proteomics in neurological disorder research is the discovery and validation of protein biomarkers. Biomarkers are measurable indicators of biological processes or disease states and play a crucial role in diagnosis, prognosis, and treatment monitoring. Proteomic studies aim to identify proteins whose expression levels or modifications are altered in response to neurological diseases. These candidate biomarkers are rigorously validated using biochemical and clinical assays to ensure their reliability and specificity.
Case Studies:
Alzheimer's Disease (AD)
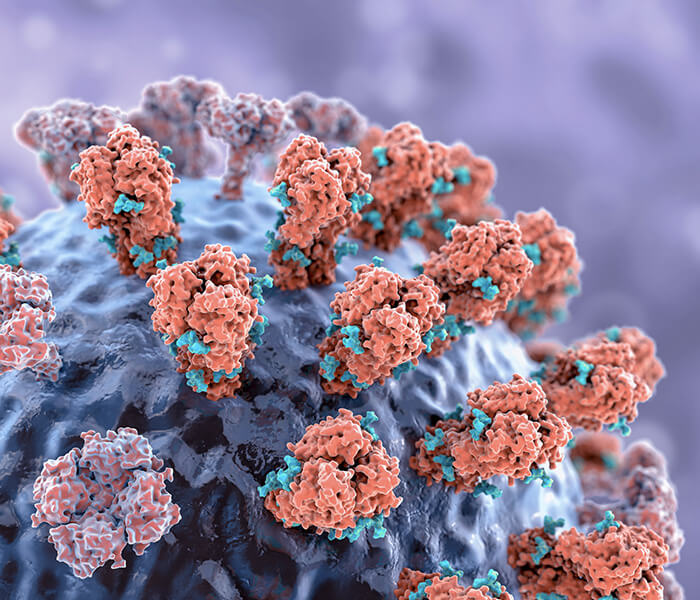
Alzheimer's Disease (AD) is a progressive neurodegenerative disorder characterized by cognitive decline, memory loss, and behavioral changes. The pathogenesis of AD is primarily associated with the accumulation of amyloid-beta plaques and neurofibrillary tangles composed of hyperphosphorylated tau protein in the brain. Proteomics has played a crucial role in identifying biomarkers that can aid in the early diagnosis and monitoring of AD.
- Amyloid-Beta (Aβ): Amyloid-beta peptides, particularly Aβ42, are considered hallmark biomarkers of AD. These peptides aggregate to form amyloid plaques, which are toxic to neurons. Elevated levels of Aβ42 in cerebrospinal fluid (CSF) and blood have been correlated with AD pathology. Mass spectrometry-based proteomics has enabled the precise quantification of Aβ42, facilitating its use as a diagnostic biomarker.
- Tau Protein: Tau protein, which stabilizes microtubules in neurons, becomes hyperphosphorylated and forms neurofibrillary tangles in AD patients. Proteomic techniques have identified specific phosphorylated tau epitopes (e.g., p-tau181, p-tau217) that are significantly elevated in AD. These phosphorylated tau species serve as biomarkers for both the diagnosis and staging of AD, with their levels correlating with disease severity.
The validation of these biomarkers involves extensive research to confirm their specificity and sensitivity. Techniques such as enzyme-linked immunosorbent assay (ELISA), immunoprecipitation, and western blotting are employed to validate proteomic findings. Clinical studies have demonstrated that combining Aβ42 and phosphorylated tau levels in CSF provides a highly accurate diagnostic tool for AD, with sensitivity and specificity rates exceeding 90%.
Recent proteomic studies have focused on identifying AD biomarkers in blood, offering a less invasive alternative to CSF analysis. Advanced mass spectrometry and immunoassays have identified promising blood biomarkers, such as plasma Aβ42/Aβ40 ratio and phosphorylated tau, which could revolutionize AD diagnosis and monitoring.
Parkinson's Disease (PD)
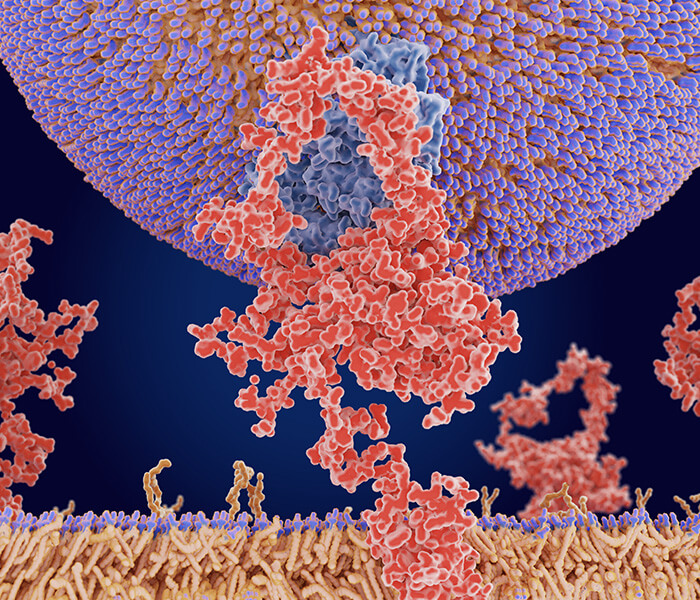
Parkinson's Disease (PD) is a neurodegenerative disorder characterized by motor symptoms such as tremors, rigidity, bradykinesia, and postural instability, as well as non-motor symptoms like cognitive impairment and autonomic dysfunction. The pathological hallmark of PD is the presence of Lewy bodies, which are intracellular aggregates of alpha-synuclein protein. Proteomic research has focused on identifying biomarkers that reflect the underlying pathophysiology of PD.
- Alpha-Synuclein: Alpha-synuclein is a key protein implicated in PD. In its aggregated form, it constitutes the main component of Lewy bodies. Proteomic analyses have identified various forms of alpha-synuclein, including total alpha-synuclein, oligomeric alpha-synuclein, and phosphorylated alpha-synuclein, which are potential biomarkers for PD. Elevated levels of phosphorylated alpha-synuclein in CSF and blood have been associated with PD.
- DJ-1: DJ-1 is a protein involved in oxidative stress response and neuroprotection. Proteomic studies have shown that levels of oxidized DJ-1 are increased in the CSF of PD patients, making it a potential biomarker for early diagnosis. Additionally, changes in DJ-1 levels in blood have been explored as a non-invasive diagnostic marker.
The validation of PD biomarkers involves multiple steps, including replication studies in independent cohorts and the development of robust assays. Immunoassays, such as ELISA and multiplex assays, are commonly used for biomarker validation. Clinical studies have shown that combining alpha-synuclein and DJ-1 measurements in CSF and blood improves the accuracy of PD diagnosis and aids in distinguishing PD from other neurodegenerative disorders.
Recent proteomic research has focused on developing multi-biomarker panels that combine several protein biomarkers to enhance diagnostic accuracy. For instance, a panel including alpha-synuclein, DJ-1, and neurofilament light chain (NfL) has shown promise in distinguishing PD from other parkinsonian syndromes.
 Putative pathogenic pathways underlying CSF biomarkers of PD (Parnetti et al., 2013)
Putative pathogenic pathways underlying CSF biomarkers of PD (Parnetti et al., 2013)
Applications of Metabolomics in Neurological Disorder Research
Metabolomics, the comprehensive study of small molecules (metabolites) within biological systems, offers unique insights into the metabolic alterations associated with neurological disorders. By analyzing the metabolic profiles of tissues, biofluids, or cells, metabolomics enables the identification of disease-specific biomarkers, elucidation of pathophysiological mechanisms, and discovery of novel therapeutic targets.
Metabolomics Techniques
Nuclear Magnetic Resonance (NMR) Spectroscopy: NMR spectroscopy is a powerful technique that provides information about the structure and quantity of metabolites in a sample. By applying a magnetic field, NMR detects signals from various metabolites, allowing for their identification and quantification. This method is non-destructive and requires minimal sample preparation, making it suitable for analyzing biofluids like blood, urine, and cerebrospinal fluid. In neurological research, NMR spectroscopy helps elucidate metabolic alterations in disorders such as Alzheimer's disease and multiple sclerosis.
Mass Spectrometry (MS): Mass spectrometry is widely used in metabolomics due to its sensitivity and specificity. It measures the mass-to-charge ratio of ions to identify and quantify metabolites. Several variations of MS are employed in metabolomic studies:
- Gas Chromatography-Mass Spectrometry (GC-MS): GC-MS is used to analyze volatile and semi-volatile compounds. It combines the separation capabilities of gas chromatography with the detection power of mass spectrometry. This technique is particularly useful for studying metabolites involved in energy and lipid metabolism.
- Liquid Chromatography-Mass Spectrometry (LC-MS): LC-MS is ideal for analyzing a wide range of metabolites, including those that are not volatile. It is highly versatile and can be used to study complex biological samples, providing detailed metabolic profiles.
- Capillary Electrophoresis-Mass Spectrometry (CE-MS): CE-MS combines capillary electrophoresis with mass spectrometry to separate and analyze metabolites based on their charge and size. This technique is effective for studying ionic and polar metabolites.
Other Techniques:
- High-Performance Liquid Chromatography (HPLC): HPLC is used to separate and quantify metabolites in a sample. When coupled with various detectors, such as ultraviolet (UV) or MS, it provides detailed information about metabolite concentrations and compositions.
- Fourier Transform Infrared Spectroscopy (FTIR): FTIR measures the infrared absorption of metabolites, providing information about their molecular structure and composition. It is useful for studying complex mixtures of metabolites in biological samples.
Discovery and Validation of Metabolic Biomarkers
Metabolic biomarkers are essential for diagnosing and understanding neurological diseases. Discovering these biomarkers involves analyzing the metabolic profiles of patients and identifying significant changes associated with specific conditions. Validation processes ensure these biomarkers are reliable and applicable in clinical settings.
Case Studies
Depression
Depression is a common yet complex mood disorder characterized by persistent feelings of sadness, loss of interest, and a range of emotional and physical problems. Understanding its biochemical basis is crucial for developing effective diagnostic and therapeutic strategies. Metabolomic profiling has played a pivotal role in identifying potential biomarkers and metabolic pathways involved in depression.
- Amino Acid Metabolism: Alterations in amino acid metabolism have been consistently observed in individuals with depression. Tryptophan, an essential amino acid and precursor to serotonin (a key neurotransmitter involved in mood regulation), has been found at lower levels in depressed patients. Reduced tryptophan availability can lead to decreased serotonin synthesis, contributing to depressive symptoms. Studies using metabolomics have identified not only decreased tryptophan but also changes in other amino acids such as phenylalanine and tyrosine, which are involved in the production of catecholamines like dopamine and norepinephrine, both crucial for mood regulation.
- Neurotransmitter Pathways: Metabolomic studies have highlighted disruptions in neurotransmitter pathways in depression. Besides serotonin, metabolites associated with the GABAergic and glutamatergic systems have shown significant alterations. For instance, elevated levels of glutamate, an excitatory neurotransmitter, and altered levels of GABA, an inhibitory neurotransmitter, have been linked to depression, suggesting an imbalance in excitatory-inhibitory neurotransmission.
- Lipid Metabolism: Lipidomics, a branch of metabolomics focused on the comprehensive analysis of lipids, has revealed significant changes in lipid profiles in depressed individuals. Changes in phospholipids, sphingolipids, and cholesterol metabolism have been implicated in the pathophysiology of depression. These lipids are essential components of cell membranes and play critical roles in signal transduction and brain function.
Validation of these findings involves rigorous clinical and biochemical assays. For example, clinical studies measuring blood levels of tryptophan and serotonin metabolites, combined with psychiatric assessments, are used to validate their relevance as biomarkers for depression. Such validated biomarkers could lead to the development of diagnostic tests that identify depression early, allowing for timely and targeted therapeutic interventions.
Schizophrenia
Schizophrenia is a severe mental disorder characterized by distorted thinking, perceptions, emotions, language, sense of self, and behavior. The complex etiology of schizophrenia involves genetic, environmental, and neurochemical factors. Metabolomics has significantly advanced our understanding of the metabolic disruptions associated with schizophrenia.
- Energy Metabolism: Metabolomic studies have consistently shown abnormalities in energy metabolism in schizophrenia. Changes in metabolites related to the tricarboxylic acid (TCA) cycle, glycolysis, and oxidative phosphorylation indicate mitochondrial dysfunction and altered energy production. For example, altered levels of lactate, pyruvate, and citrate have been observed in patients with schizophrenia, suggesting disruptions in cellular energy metabolism.
- Oxidative Stress: Elevated oxidative stress and impaired antioxidant defense mechanisms are critical features of schizophrenia. Metabolomic analyses have identified increased levels of oxidative stress markers, such as malondialdehyde (MDA) and reduced levels of antioxidants like glutathione (GSH). These findings support the hypothesis that oxidative damage contributes to the pathophysiology of schizophrenia.
- Neurotransmitter Pathways: Similar to depression, schizophrenia involves significant alterations in neurotransmitter pathways. Metabolomic studies have highlighted disruptions in the glutamatergic, GABAergic, and dopaminergic systems. Elevated levels of glutamate and altered GABA levels have been consistently observed, pointing to an imbalance in excitatory and inhibitory neurotransmission. Additionally, changes in metabolites related to dopamine metabolism, such as homovanillic acid (HVA), have been implicated in the disorder.
Validation of these metabolic biomarkers involves comprehensive clinical studies. For instance, measuring oxidative stress markers and antioxidant levels in patients with schizophrenia can help establish their relevance as diagnostic and prognostic biomarkers. Metabolomic profiles combined with clinical assessments and genetic data can provide a more holistic understanding of the disease, paving the way for personalized treatment approaches.
Reference
- Parnetti, Lucilla, et al. "Cerebrospinal fluid biomarkers in Parkinson disease." Nature Reviews Neurology 9.3 (2013): 131-140.